Do the NIH and WHO COVID treatment recommendations need to be fixed ?

This article was originally published on trialsitenews.com and is crossposted by kind permission of Steve Kirsch.
Executive Summary
This is the first in a series of articles arguing that obeisance to constrictive evidence-based medicine (EBM) treatment protocols in a pandemic is causing an unnecessary loss of hundreds of thousands of lives.
If, instead of exclusively relying on EBM for developing treatment recommendations, we made medical decisions based on looking at all the available evidence and 1) made recommendations, which are most consistent with the evidence to date, 2) made recommendations that are more likely than not to save the most lives, and 3) considered the costs of being wrong (death vs. minor temporary side effects), then we would arrive at a completely different set of recommendations. We would not be afraid to make mistakes because we would be seeking to minimize the loss of life.
There is abundant evidence that COVID is best treated as early as possible with a cocktail of drugs, two of the most effective and safest being fluvoxamine and ivermectin. Doctors uniformly report that the earlier a patient is treated, the better the outcomes. I have yet to hear of a case where a patient who was treated within 24 hours of first symptoms with those two drugs needed to be hospitalized or developed any long-haul COVID symptoms.
I believe that a major reason why we have so many hospitalized COVID patients is that patients are told to do exactly the opposite of what they should be doing: if they don’t qualify for the monoclonal antibodies, we tell them to stay home and do nothing unless they get really sick. When patients present late, they are much more difficult to treat and the outcomes are never as good. If there is a fire in the kitchen, would you wait until your whole house is on fire before you called the fire department? Sadly, this is exactly what many patients are doing in India right now, waiting as many as 9 days after first symptoms before seeking treatment.
And when a patient finally presents for treatment, doctors have been reluctant to prescribe the two most effective drugs because current recommendations of the NIH and WHO for these drugs are either neutral or negative and these recommendations strongly influence their local guidelines.
The NIH and WHO recommendations are made by evaluating clinical studies, but they fail to take into account the costs of being wrong. If a drug has little to no side effects, and consistent evidence of a lifesaving benefit, why not give that drug the benefit of the doubt even if the evidence quality is low? If we are wrong, there is no harm. If we are right, we can save an enormous number of lives.
This article examines the evidence for three drugs in detail: hydroxychloroquine, ivermectin, and fluvoxamine. In every case when these drugs are used early in the disease, all the evidence (studies as well as results in clinical practice) is consistently positive, yet the official recommendations are either NEUTRAL or AGAINST their use. If the drugs don’t work, how do they explain all the evidence? They don’t. It is a mystery left for the reader to solve.
Fluvoxamine has shown 100% effect sizes in two very high quality randomized trials (one a DB-RCT, the other real-world quasi-randomized), both published in top peer reviewed journals. If fluvoxamine doesn’t work then why were none of the 77 patients in the Seftel study who opted for the drug hospitalized (vs. 12.5% of the no treatment group). Why did none of the treated patients develop long haul COVID compared to a 60% long-haul rate in the healthier group that declined treatment? Not only are these agencies unable to tell us the true cause of these important observations, they appear to have no interest at all in finding out what the actual cause was; they simply assumed it must have been experimental bias or a confounder or two. I offered $1M to anyone who could explain the observed outcome if it wasn’t due to the drug and nobody took my money. So the only explanation left is that the drug actually works really well when it is given sufficiently early. At no time was I ever worried I’d lose the challenge. For fluvoxamine there is only 1 chance in 1e14 that the long-haul effects observed could have happened by chance (10 orders of magnitude more certain than the vaccine).
On January 22, 2021, a key opinion leader panel of 30 experts from the CDC, NIH, and top US academic centers met to review the evidence and recommended by more than a 2:1 ratio that doctors talk to their patients about fluvoxamine for COVID. That expert advice is mostly ignored by doctors; clearly the NIH guidelines trump expert opinion.
Sadly, many doctors don’t like to use drugs that are still in clinical trials, so they will wait another 6 months to a year or more for the trials to finish just to be sure, even if there are no other drugs available. Patients will die, but the physician doesn’t want to make a wrong decision, even if there is minimal downside if they are wrong.
There are 29 studies of HCQ (six of them RCT) and all are positive, yet somehow this results in an AGAINST recommendation from both organizations.
For ivermectin, there are now 6 systematic reviews. Systematic reviews are the highest level of evidence in EBM and all of these reviews recommended FOR ivermectin (5 are published, 1 is awaiting publication). If 6 out of 6 positive systematic reviews are not enough, what is it going to take to get a positive recommendation from these organizations? How high is the bar? To this day, none of us has any clue. They won’t tell us. Were there errors in these systematic reviews? Neither agency has pointed out any such errors.
Recently, fifteen days after Goa India authorized the use of ivermectin, the number of patients needing hospitalization dropped 58%. If the drug doesn’t work (or is as harmful as the WHO claims), then what DID cause the fall in cases there? There are many many more examples.
Ideally, the NIH and WHO recommendations should tell everyone to be treated ASAP after infection with known effective drug combinations and dosages. If there is a better combination than ivermectin and fluvoxamine, these agencies should suggest the better combo. If we made just this one simple change in what we tell patients, hospitals worldwide would empty out.
Both the NIH and WHO have declined to defend their recommendations in a neutral debate. The NIH even refuses to disclose if there was a vote on their ivermectin recommendation.
Does anyone remember what the WHO said on March 13, 2020 about how to treat Ebola? Their advice, delivered by Dr. Michael J. Ryan, was spot on:
- “You need to react quickly. Be fast. Have no regrets. You MUST be the first mover”.
- “The virus will always get you if you do not move quickly.”
- IF YOU NEED TO BE RIGHT BEFORE YOU MOVE – YOU WILL NEVER WIN”.
- PERFECTION IS THE ENEMY OF THE GOOD WHEN IT COMES TO EMERGENCY RESPONSE MANAGEMENT.
- SPEED TRUMPS PERFECTION.”
- “Everyone is afraid of making a mistake. Everyone is afraid of the consequence of error, BUT THE GREATEST ERROR IS NOT TO MOVE.
- THE GREATEST ERROR IS TO BE PARALYSED BY THE FEAR OF FAILURE.”
Needing more evidence from a large, double-blinded, cumbersome randomized phase 3 trials that will take months, if not years, to finish is inconsistent with the WHO’s original message above. For example, one year later, HCQ, ivermectin, and fluvoxamine are still waiting for their definitive phase 3 trials and outpatient clinical studies of promising drugs such as camostat still haven’t completed enrollment. If only the WHO would heed their own advice from a year ago, we’d have had a completely different outcome today with COVID.
The bottom line is that while both the NIH and WHO have a laudable history of delivering good advice, they aren’t infallible.
The Ebola advice from the WHO was right on point and applicable to COVID: we must treat this virus early and we must not be afraid to use the drugs which today show the best evidence.
Over three million people have lost their lives to COVID, yet the drugs that could have prevented most of those deaths have been sitting on the shelf the entire time. We have been afraid to use them as we await more and more data from trials, all of which are turning out the same way showing these drugs are both extremely safe and effective. We are afraid of making a mistake. To avoid further loss of life, each country should immediately re-examine the evidence and make their own recommendations based on the principle of all the available evidence. That is the best way to minimize the number of lives lost.
India, Brazil, and most other countries all rely on COVID treatment guidance from the two organizations that people most trust for medical advice, the National Institutes of Health (NIH) and the World Health Organization (WHO).
Yet following the COVID guidance of these organizations is failing to prevent the unnecessary death of millions of people worldwide.
Is the guidance provided by these organizations correct? Or is there a possibility it could be harmful to follow their guidance?
This is now a matter of urgent public interest because India recently adopted ivermectin as standard of care for early treatment of COVID, which is exactly opposite to the WHO recommendation.
Is India doing the right thing? Or are they making a huge mistake? It’s important that people around the world hear from experts from both sides so they can decide for themselves.
Individual states in India can issue their own guidance. Goa wants people to take ivermectin, but Tamil Nadu just decided it should not be used. Who is right?
To help resolve this issue, TrialSiteNews has asked the WHO and NIH to provide experts for an open debate with the world experts on these drugs and a mutually agreeable moderator in a live zoom meeting which will be recorded and posted to TrialSiteNews and YouTube for the world to reference.
In the meantime, in this op-ed, I will explain why it is more likely than not that the NIH and WHO have missed the mark on three important drugs: hydroxychloroquine, ivermectin, and fluvoxamine and why world governments should ignore their guidance and independently evaluate the evidence.
This is a long article. Very long. But this is an important topic because over 3M people have lost their lives to COVID so far and the longer we fail to act on the clear evidence in plain sight, the more people will lose their lives unnecessarily. So please bear with me as I tell an important story that needs to be told.
The case for hydroxychloroquine
Let’s start with hydroxychloroquine (HCQ) for use in early treatment, i.e., immediately after you are diagnosed with COVID. Both organizations recommend AGAINST using hydroxychloroquine for early treatment after infection, even though there isn’t a single published study that supports their recommendation.
As of May 7, 2021 there have been 29 studies of HCQ for early treatment – all with zero negative results for the most serious outcome reported. The average risk reduction for the most serious outcome reported in these trials was 65%. Here’s a chart from c19hcq.com that shows this:

Skeptics might argue the reason all the studies are positive is that journals are more likely to publish positive results than negative results. But in fact, there is a good argument that the bias is the reverse for HCQ, where negative studies are more likely to be published than positive studies. But in this case, those arguments don’t matter as the skeptics can’t point to a negative early treatment trial that has not been published so the debate is moot.
Now, let’s talk safety. HCQ is on the WHO list of essential medicines, i.e., one of the safest and most effective drugs in a health system. Lupus patients are put on HCQ and remain on the drug for life. The drug was FDA-approved more than 65 years ago. In 2016, it was the 135th most-prescribed medication in the United States, with more than 4 million prescriptions. Dose escalation studies in lupus patients and in rheumatoid arthritis patients established that 800 mg per day for life and 1,200 mg per day for 6 weeks are extremely well-tolerated.
The WHO says HCQ is safe to take for autoimmune diseases or malaria. However, they admit that there is weak evidence supporting their contention that HCQ is unsafe to take for COVID. But the problem with this is 1) they admit that the certainty of the evidence is “low” to “very low” and 2) they don’t break it out by the disease phase. We are interested in early treatment, not late treatment. You can’t just lump all the studies into one analysis.
In order to see what is actually happening in early treatment patients when they take HCQ, I reached out to Brian Tyson and George Fareed, whose practice has used HCQ in treating more than 6,000 people of all ages with COVID. The risk of diarrhea and nausea/vomiting claimed by the WHO is both “very rare and very minimal.” In general, diarrhea is more likely to be caused by COVID than the drug. Fareed said he has had “zero cardiac issues” with any patients. They have never had any reason to drop HCQ from their treatment protocol and I don’t know of any physician in the US who has a lower rate of hospitalization for COVID than Tyson and Fareed. If the WHO is right, then how do they explain this anomaly? Tyson and Fareed certainly didn’t get lucky on 6,000 patients and the average age of their patients is 60 years old.
So the bottom line so far is 29 studies all positive, and real-world evidence on thousands of cases is also consistent with the studies. Our hypothesis that the drug is effective is consistent with the data. But the WHO and NIH say we should not use this drug, yet have no plausible explanation for the consistently positive data.
Some scientists will cite the HCQ analysis published in Nature which definitively shows that HCQ is harmful. But that was a meta analysis, which heavily weighted studies of high dose HCQ given to very late stage hospitalized patients. No early treatment outpatient trials were included. The paper says “Findings have unclear generalizability to outpatients, children, pregnant women, and people with comorbidities.” I agree!
I’m not arguing for high dose HCQ in late-stage hospitalized patients. That’s a losing proposition. As you can clearly see, all the early treatment results are all positive (top graph) whereas if you look at all stages, that’s when the negative results occur, so it is very important to pay attention to segregating the data when doing meta-analyses.
Here’s a simple analogy as to why drug timing makes a huge difference: a small bucket of water works great if the fire is small (early stage). After the house burns down, the same bucket of water will do nothing to repair the damage, even if we increase the amount of water, and will probably further damage any remains.
Other scientists might reference the fact that the FDA revoked the EUA on HCQ, but the revocation was based on studies on hospitalized patients, not outpatients. So that argument doesn’t hold water.
Finally, some people may reference the Skipper study, an outpatient HCQ early treatment trial that concluded that “hydroxychloroquine did not substantially reduce symptom severity in outpatients with early, mild COVID-19.” I know a few things about that particular study because I was one of the “private donors” who funded it. If you look at each metric they looked at, the cohort who got the HCQ always did better. See this analysis for details. There is much more to this study that will come out later that will show that HCQ works even better than the 51.7% drop in hospitalization rate reported in the paper.
In short, HCQ is both effective and safe for early treatment at dosages of 600mg per day and more. If anyone tells you otherwise, please ask them for both clinical studies and real-world evidence to back up their claim. At that point, they will say that they don’t have time to talk to you and walk away. This happens to me all the time. It’s frustrating.
The case for ivermectin
Now let’s look at ivermectin for early treatment of COVID.
The NIH says it cannot figure out whether ivermectin works or not, so they give it a NEUTRAL rating.
The WHO and EMA recommendation for ivermectin is: DO NOT USE (except in a clinical trial).
Here is a summary of the 20 early treatment studies on ivermectin done by 184 authors from c19ivermectin.com.
All 20 studies are positive in the most serious effect reported. I am not claiming that all studies were statistically significant; they weren’t because these were small studies with relatively few “events” so even for large effect sizes, it’s hard to get statistical significance. However, six were statistically significant in isolation.
Let’s take the worst case, and consider the argument assuming each study is statistically insignificant. Some people might argue you can’t conclude anything from any study: 20 x 0 = 0 and there is no conclusion. Furthermore, they would argue you cannot combine the data since each study was different. Therefore we can conclude nothing.
That sounds logical, but it’s wrong.
Ivermectin was the common element in each study. The dosings were different and the comparator groups were different, but in all 20 tests, the cohort with the ivermectin emerged victoriously. That’s very unlikely to happen by chance. It’s like what would happen if you added Michael Jordan to any NBA team and see if he’d make a difference. You know exactly what would happen.
If the drug were completely neutral as the NIH believes, then the chance of all the studies being positive is 1 in 220 which is one in a million. In other words, it’s very unlikely the drug is neutral.
Nobody can claim “publication bias” where positive studies are more likely to be published than negative studies because NOBODY has been able to find any ivermectin studies that completed and were negative that have not been published.
Here’s an analogy: suppose I gave a single coin to 20 people (one at a time consecutively) and each person flipped it just one time and every time it landed on heads. Well, each of those 20 studies would be statistically insignificant alone since each person flipped it just once. Then I tell you that the coin is either weighted on one side or is a fair coin. If you get the answer right, you win $1M. I think anyone who is asked that question would say the coin was weighted because they would be correct 999,999 times out of 1,000,000. However, the NIH and WHO would look at each of these trials as insignificant alone, and thus in their mind 20×0=0 so there is nothing to conclude and they would be equally likely to bet head or tails.
But the WHO isn’t saying that the drug is neutral. They are recommending people NOT use ivermectin (except in a clinical trial). So they are concluding that the net benefit is negative — exactly opposite of what the evidence shows.
If the WHO is right and ivermectin is causing great harms, and the NIH is right that the drug does absolutely nothing, then how can they explain these observations:
- Mexico encourages the widespread use of ivermectin and their hospitals are nearly empty. If it wasn’t the ivermectin, how did this miracle occur? We’re not talking about a single hospital here; we’re talking about virtually every hospital in Mexico.
- How can Fareed and Tyson treat over 6,000 COVID patients using HCQ and ivermectin with close to a zero hospitalization rate? Both drugs make things worse according to the WHO.
- The peaks and valleys of the fatality rates in countries such as Peru, Mexico, and Zimbabwe are correlated with the distribution and revocation of ivermectin. If it wasn’t the ivermectin distribution and revocation that caused these effects, then what was the real cause?
- This study just released in Mexico with over 200,000 people showing a drop in hospitalizations of over 52% among those who took the ivermectin treatment kit. If it wasn’t the treatment kit, then what was it?
- The BIRD systematic review done by an international panel of experts looked at all the data and concluded that ivermectin should be deployed. If this review is wrong, why hasn’t anyone exposed the errors? There are no papers in the published literature or on any pre-print server anywhere in the world pointing out any flaws in the study. Why is that?
- The Kory comprehensive narrative review of the emerging evidence supporting ivermectin passed peer review at two different journals (a rare event) and concluded that ivermectin is effective in all stages of COVID. So if their conclusions were flawed, how could three senior governmental scientists tasked with the peer review have accepted the paper? Note: that after the management of Frontiers decided to censor Kory’s paper, the entire group of guest editors appointed by Frontiers resigned en masse citing the journal’s rejection of Kory’s paper as scientific misconduct. This is important because the misconduct they were objecting to was not by Dr. Kory, but by the management of the journal.
- Uttar Pradesh Health Officials on Record: Ivermectin as Prophylactic Has Lowered COVID-19 Infection Rate & Death Rates. A government pronouncement and nobody is disputing it. If they got it wrong, then what’s the real cause?
- Whatever happened to Andrew Hill? Why did he drop from sight after initially recommending ivermectin? Hill was commissioned by the WHO to do an objective study on ivermectin. He concluded that it was on average 75% effective (anywhere from 48% to 88% improvement is the 95% confidence interval), and subsequently agreed to have his conclusion re-written by the study sponsors so that it recommended that more evidence was needed, and has now dropped from sight and isn’t talking to anyone. What happened to Dr. Hill and why did he drop from sight?
- If the drug doesn’t work, then how does one explain the highly statistically significant dose-response relationship in at least one DB-RCT? For example, Ivermectin shows clinical benefits in mild to moderate COVID19: A randomized controlled double-blind, dose-response study in Lagos which concludes that “The Days to COVID negativity [DTN] was significantly and dose-dependently reduced by IV (p = 0.0066).” This is tough to explain since the p-value is so low, nobody can argue that they just “got lucky.” How could you get such a low p-value if the drug doesn’t do anything? Further, Dr. Hill reported that in 10 of 13 randomized trials a statistically significant impact on the time to viral clearance was found, with larger impacts reported among the multi-day dosing trials than on the single-day. Again, more evidence of a profound dose response. That cannot happen if the drug doesn’t work.
- If the drug doesn’t work, then why do all physicians who prescribe the drug in the real world all report drops in hospitalization rates? Is there a case of a doctor anywhere in the world who started prescribing ivermectin and then stopped giving it because it didn’t decrease the doctor’s hospitalization rate?
- Scientists at AIMS in India did a systematic review of the ivermectin data. As noted in the figure below, systematic reviews are the highest level of evidence in the evidence-based medicine pyramid, the “Gold Standard.” They found that “adding ivermectin led to significant clinical improvement compared to usual therapy (OR=1.98, 95% CI: 1.11 to 3.53, P=0.02).” They noted that the quality of the evidence was “very low,” but that’s what we have to work with today. So where is the high-quality evidence that shows the opposite to justify the WHO’s position? And how do we explain the statistically significant agreement in all these low-quality studies?

If you believe ivermectin is a danger, you need to explain the true cause of all 11 of these anomalies. If you can’t even explain one of them, then why should anyone take you seriously? After all, those with the opposite viewpoint can explain every single one of them. In seconds.
A study many people focus on as proof ivermectin doesn’t work is the López-Medina study published in JAMA. It determined that healthy patients recovered 20% faster taking ivermectin. Yet, the conclusion was that it shouldn’t be used because there the effect did not reach statistical significance. If anyone says the Lopez study was a well-done study, you can point them to this page which summarizes the findings of the study. It shows that for every metric in the study, the ivermectin group did better. If the drug doesn’t work, how do they explain the consistency? Sure, none of these effects was statistically significant, but they were all positive (just like the effects in the other studies). The lack of statistical significance just means the study was underpowered because there were too few “events.” This is what happens when you do a small study with younger patients. Finally, point these people to this analysis and ask them to point out flaws in the paper that pointed out flaws in the Lopez study.
As for safety, ivermectin has a well-established safety profile. Research shows the drug is safe at a wide range of dosages and treatment duration. Various WHO documents on parasitic infections refer to ivermectin’s “long safety record.” A search of reported adverse event profiles in pharmaceutical databases including the United States VAERS and the WHO’s Vigiaccess find that ivermectin is one of the safest medicines in history, and has been distributed widely by the WHO across many continents in children, pregnant women, and adults, and is thus on the WHO’s List of Essential Medicines. I was unable to find a reported death from an overdose of Ivermectin, whether intentional or accidental, with almost 4 billion doses having been prescribed.
The FDA says horse ivermectin is unsafe for people. Yet, no one is recommending people take horse ivermectin. The FDA says large doses are unsafe and no one appears to be recommending any dose that exceeds the ranges studied in the existing trials.
In summary, all the studies for early treatment have the group with the ivermectin doing better than the group without the ivermectin, all the anecdotal data is positive, and there is no new evidence that ivermectin is suddenly unsafe for consumption.
Therefore, taking the position that ivermectin should be used for early treatment is likely to save more lives than taking a position to avoid use of the drug. This isn’t a close call. There is no way you can justify the WHO or NIH position.
The case for fluvoxamine
The WHO is so out of touch with the latest research that fluvoxamine hasn’t even made it on to its list of potential drugs to treat COVID:
Go to c19early.com and look at the chart. Fluvoxamine is the #1 approved drug on the list. It’s cheap, safe, widely available, and effective. But it doesn’t even merit inclusion on the WHO list. I tried to bring this omission to their attention, but they requested I stop bothering them.
The NIH is better; it is listed on the NIH’s COVID Treatment Guidelines, and the NIH knows that there have been two quality randomized trials done by top US researchers (one trial was a DB-RCT, the other was quasi-randomized which the NIH categorizes as “observational” but that’s a debate for another op-ed), both were published in peer-reviewed journals, and both papers were given a prestigious “Editor’s Choice” designation.
In other words, fluvoxamine has something that ivermectin and HCQ both lack: two quality studies, done by highly respected researchers associated with top-quality institutions, published in top peer-reviewed journals, both studies had statistically significant results on a critical clinical endpoint (hospitalization), both were an interventional trial, both were randomized, and both studies were highlighted by the editors. It is for these reasons that the mainstream scientific community believes that the case for fluvoxamine is superior to the case for ivermectin and HCQ.
Of the most respected scientists I know, 100% would choose fluvoxamine in a heartbeat over the other two drugs if they got COVID and had to pick a treatment based on the evidence available today. A top medical school looked at fluvoxamine and other options and the consensus was that the case for fluvoxamine was clearly the strongest. I also know of a DB-RCT study, not yet published, which compared the efficacy of fluvoxamine against ivermectin and fluvoxamine had the greater benefit by far.
The consistent superior rating by mainstream scientific experts is important because if a country adds ivermectin and/or HCQ to their treatment recommendations, then adding fluvoxamine should be a “no brainer.” Unfortunately, this isn’t the case today, anywhere in the world. However, the FLCCC did add fluvoxamine to their early outpatient treatment guidelines based on the evidence and the experience with doctors all over the world with the combination.
The first fluvoxamine study (Lenze), published in JAMA, had 100% effect size in protecting against hospitalization criteria defined as respiratory distress (since that’s what most people get hospitalized for and they didn’t want to count it if you got hit by a truck and got hospitalized). None of the 80 patients on fluvoxamine met the clinical endpoint vs 8.3% of the 72 that got the placebo. That’s an effect size of 100%, i.e., impossible to beat.
But, the numbers were small and the study was deemed as “hypothesis generating.”
One professor noted that “the authors of that study concluded that their results were more hypothesis-generating than a clear call that this is an effective treatment.” Well of course! If you don’t say that in your paper, you can’t get it published in JAMA. Do the authors really believe that? Of course not. But you’ll have to take my word on that part because if you ask them publicly, they will toe the party line and say exactly what they are expected to say.
The JAMA paper didn’t generate a hypothesis that fluvoxamine might work for COVID. The hypotheses were generated by many independent researchers who looked at the SSRI data and noticed that these people had a remarkably lower rate of hospitalization and death than their matched peers. And the Washington University study itself was based on a University of Virginia study demonstrating that fluvoxamine reduces inflammation in sepsis. Dr. Reiersen speculated that it might work in COVID. She generated the hypothesis and she created the study that confirmed her hypothesis. So we didn’t just get lucky here… the JAMA study confirmed hypotheses made by others from three different countries using different studies.
What is even more remarkable is that, in the fluvoxamine confirmation study by Dr. Seftel at Golden Gate Fields which started the day after the JAMA paper was published, patients were able to choose whether they were treated with the drug or not and the sicker patients opted for the drug. Also, there were eight patients who initially rejected treatment, developed symptoms, and then asked to be placed in the treatment group. So this trial wasn’t random: it was WORSE than random; we should have expected that the treatment group would have really bad outcomes because of this bias.
But the opposite happened: 100% of the 77 patients who received the drug recovered to normal in an average of 3 days and demanded to get back to work vs. a 12.5% hospitalization rate of the patients who refused treatment. That’s a p-value of .0026.
Therefore, anyone who dismisses this study by saying “it wasn’t randomized” is missing the point. The results of this trial are stronger than the JAMA results: the p-value is stronger, the randomization was more “challenging”, and the physician had direct access to every patient. Also, the drug was administered promptly after the PCR test came back positive, a key factor in the 100% success of the trial.
So now we have two studies with 100% effect size, each with p value <.01. What do you think the chances are that it won’t be confirmed in a phase 3 trial? I’d say there are basically only two chances it won’t be confirmed: slim and none.
But here’s the more impressive observation that was noted in the Seftel paper that NOBODY looked at is that none of the 77 patients treated with fluvoxamine developed any long-haul COVID symptoms compared to 60% of the patients in the no-treatment group. Nobody has yet stepped forward to successfully explain, if the drug doesn’t work, how this could occur. It certainly wasn’t likely to happen by chance. The odds of it happening by chance is 1 in 1014, i.e., next to impossible. There is no statistical fragility here. This is an impossible result if the drug doesn’t work.
Lastly, Dr. Seftel used a dosage of the drug, 50mg BID x 14d, that is one-third of the FDA authorized dose (and the maximum dose used in the Lenze study). Even with such a small dose, patients uniformly were better in 24 hours and most were back to normal in 3 days. The lower dosing was extremely well tolerated with no reported side effects from the drug. Zero.
So to summarize so far, we have an inexpensive drug with a 37-year safety record, given at 1/3 the FDA authorized dose that has no side effects (for the vast majority of patients), that was 100% effective in preventing hospitalization, death, and any long-haul COVID symptoms. What’s not to like about that? If there is an approved drug that has multiple high quality studies, all statistically significant clinical endpoints with better results, we should use that. If not, why shouldn’t we be giving people fluvoxamine now?
And then there is the data from docs who have been prescribing it. They uniformly say it works like magic. Not a single doctor who starts prescribing it stops (and I’ve seen them stop other drugs that they try and don’t work so I know they are tough to persuade). For example, Dr. Amol Kothalkar, a physician in the Buldhana district of Maharashtra, India has been using fluvoxamine in his practice for months and he swears by it and has told me on more than one occasion it is unethical for doctors not to prescribe this medication for COVID. Dr. Kothalkar is unusual because he gets regular blood work on his COVID patients so he can see the cause-and-effect between the start of fluvoxamine treatment and the rapid normalization of CRP. He knows that if can treat patients sufficiently early in the virus, all recover quickly, none are hospitalized or end up with long-haul COVID.
There is no evidence at all fluvoxamine makes COVID worse, and no doc has reported it doesn’t work. There are no neutral or negative anecdotes. There is no data you get better results by waiting. There is no data the drug benefit/risk ratio is <1 for younger patients. Indeed, all the evidence we have so far shows it helps kids very quickly kick the virus; doctors are stunned by the effect.
My favorite story involves the workers at the racetrack who at first didn’t opt in for the fluvoxamine… only about 40% followed the doctor’s advice to take the drug. But two weeks later, when the employees could see the stark contrast between the two cohorts, 100% of the employees who later got sick demanded they be put on the drug. Even the track management, who weren’t sick, asked for fluvoxamine prescriptions so in case they got sick, they could start treatment immediately. So the effect was so large, it was crystal clear to these non-experts whether the drug was working. They were not swayed by any particular analysis or study indicating a lack of bias or p-values. The reason this is significant is that because it was clear to everyone, even those not involved in the study at all (the track management), that the drug worked, it means that there wasn’t bias on behalf of the doctor.
So my question is, how can this be obvious to 100% of the workers at the racetrack that the drug works, yet the experts at NIH–with access to all the data–simply cannot figure out whether the drug is likely to work or not?
Of course the NIH would argue that they are being careful because these results could happen by chance.
Sure, all of these positive results could happen by chance… I acknowledge that there is a 1 chance in 1014 this outcome occurred by chance, but for all practical purposes, it is impossible for this to happen “by chance.”
My point is that the statistical certainty that the drug works is well beyond that required by scientists in any normal conditions. We effectively have two randomized studies with p<.01, which is more than adequate for a positive recommendation and we have an extra gift: the symptom data with p<10-14.
I’ve discussed these results with data scientists who tell me “it’s IMPOSSIBLE that the drug doesn’t work” (and then they quickly clarify that “impossible” means the chance it doesn’t work is extremely small). So to me, it is more than ridiculous that fluvoxamine has a NEUTRAL recommendation from the NIH (and not even mentioned by WHO).
I will happily retract my claim that the NIH got it wrong here if anyone at the NIH can come up with a bias or confounder that can explain the results that Seftel observed if it wasn’t the drug. It wasn’t observer bias since everyone saw the same miraculous difference and reacted the same way. And it wasn’t because the drug is anxiolytic because, when you remove anxiety from the list of symptoms, it doesn’t change the numbers. And the patients couldn’t know who was not going to be sick because if they knew that those patients would have chosen no treatment! And it wasn’t a placebo effect because there isn’t one for COVID that can eliminate all hospitalization risk and long-haul symptoms (think about it: if there was one, then everyone who enrolled in any arm of a DB-RCT would recover in 3 days and nobody would get long-haul symptoms). And finally, it couldn’t be anything about the drug itself reducing symptoms during the study because 4 months after they stopped using the drug, the treated patients still had no long haul COVID and the group that refused the drug was still suffering. All of this is verifiable but nobody has been interested in checking it out even after I offered $1M to anyone who could prove that the effect was caused by something other than the drug.
When the Covid Early Treatment Fund applied for an EUA we got rejected by the FDA saying our evidence was insufficient to get an EUA (which is a very low bar because it only requires that the FDA believes that there is evidence that the benefits outweigh the risks). So how do they explain how the Seftel study got such an amazing result? They don’t. They just totally dismissed it with a hand-waving argument that there could be observer bias or randomization issues. That’s just not plausible, but you don’t get to argue with them.
Since the world is desperately looking for a magic pill that treats COVID infections, you’d think the entire world (especially India and Brazil) would be focused on verifying whether Seftel’s study was valid or not, because if it was, we’d already have the answer: a cheap, safe pill with remarkable efficacy. So when this “miracle at the racetrack” happened, why didn’t world governments and the mainstream press get all over this either to confirm or disprove it? If they confirmed it, it would be the story of the decade. Other than 60 Minutes, nobody in the mainstream media has bothered to look into it (and we even enlisted the aid of multiple PR and media experts, including an Emmy award winning reporter, to do the outreach to the press). I note that 60 Minutes didn’t discover anything amiss or it would have been a very different story. Is investigative journalism dead? The response we got was that people were too busy to look into it and they would prefer to wait for the Phase 3 trial which will likely take another six months to complete enrollment. For an investigation that could be completed in a few days, waiting six months seems like the wrong tradeoff. Lives are lost because you don’t have a day or two to check out the story to verify its legitimacy?
So we are simply left with no other rational explanation that can fit the facts other than the drug really works. Saying it is NEUTRAL is completely unjustifiable; it doesn’t fit the facts. If it was NEUTRAL, someone would be knocking on my door to claim their $1M prize money for explaining how we were all fooled into thinking that the drug works. They would be able to explain away not just the Seftel trial, but the Lenze trial, the two observational studies in France, the one in Germany, and the two in the US (at TriNetX and Stanford/UCSF), as well as explain how doctors in multiple countries using the drug on hundreds of patients were misled into the thinking the drug was working when it was actually doing nothing. We’d have to believe that everyone who used the drug just “got lucky.”
My final point is that I’m hardly alone in believing the evidence is compelling. Any doctor who has ever prescribed fluvoxamine for COVID is a believer. A key opinion leader panel of 30 infectious disease experts from NIH, CDC, and academia met via zoom on Jan 22, 2021, to review the fluvoxamine data. They voted by more than a 2:1 margin that doctors should talk to their patients about using fluvoxamine for COVID.
Lastly, Vikas Sukhatme, Dean of the School of Medicine at Emory University and a world expert on repurposed drugs, also has called publicly for the use in fluvoxamine, most recently in an op-ed he co-authored with his wife Vidula in the Times of India.
Key question: Do we really need to wait for the perfect, definitive high quality study? I don’t think so.
I would claim that waiting for definitive high quality studies in a pandemic before making recommendations is inappropriate. Other doctors I know call it “unethical” or “criminal.”
In the case of HCQ, for example, the medical community embraced a study published in The Lancet on hydroxychloroquine which concluded that HCQ caused more harm than benefit. The first author is a professor at Harvard Medical School and it was published in a top journal. And the result confirmed what everyone thought: that HCQ didn’t work. How can you do any better than that?
There was just one problem. That study, that everyone relied on as definitive, was rapidly attacked by scientists and subsequently retracted by the journal. That’s what happens to true junk science: it gets retracted.
Conversely, none of the so-called low-quality studies showing these drugs are effective have been attacked as fraudulent or inaccurate and none have been retracted. So why shouldn’t we believe them?
It is ironic that the high-quality study that all the scientists believed, rather than the “low-quality’’ studies, was the only paper that was retracted.
Can lots of low to moderate quality studies lead us to the right answer? Yes!
The NIH and WHO would argue that lots of low-quality studies give no indication at all as to whether a drug works or not because 100*0 is still 0 or expressed another way, “garbage in, garbage out.” They will say that the plural of “anecdote” is “anecdotes” and not data. They will claim they are practicing “good science” and adhering to the principles of evidence-based medicine by only allowing high-quality data to influence their recommendations.
I respectfully disagree with their approach. As an MIT-trained engineer, I was taught how to combine evidence and how to make decisions that will have the highest statistical likelihood of optimizing outcomes.
It is patently false that lower quality evidence gives us absolutely no clue as to what is going on. All studies have flaws, but when there is such consistent agreement between all these independent studies involving hundreds of researchers, it is irresponsible to ignore what these studies are trying to tell us. Many of the ivermectin, HCQ, and both the fluvoxamine trials are high quality studies without any conflicts of interest. No one has suggested there is any collusion between these researchers or a “smoking gun.” So instead of completely ignoring these imperfect studies, we can understand their limitations and assess their likelihood of being accurate.
For example, if I have a study done by a researcher who in their last 100 studies always got the right answer, if all other factors are neutral, it’s going to be a lot more likely that this latest research paper will be accurate as well. Normally, nobody takes the time to do this analysis because it takes so long, but here the situation today is different: as of May 14, more than 585,000 Americans have died from COVID, and the Phase 3 studies that everyone is waiting for could still be six months away, or more.
I’m not going to argue that any of these studies for any of these drugs is or was perfect. They weren’t. All of them are flawed.
But I will argue that when you have a large enough effect size, even low-quality studies will show the effect.
The easiest way to understand how that can happen is with a simple example. Suppose I asked a bunch of 12-year-old kids armed with glucose meters to do a study on whether injecting insulin lowers blood sugar, I would bet that 100% of their studies would be positive. Conversely, if those same kids tested injecting a saline solution, I would expect that none of them would find an effect. So unless we believe that every single one of the hundreds of researchers and dozens of journals who published these studies are less competent than our average 12-year-old, we should believe that the results they published are a lot more likely to be correct in aggregate than they are to be wrong.
Put it another way: when was the last time we had 20 or more independent phase 2 studies, all 100% consistent in showing a positive effect and then a later phase 3 trial showed that all 20 of the phase 2 studies were wrong and there was either no effect or a negative outcome? As far as I know, that has never happened in the history of medicine.
It would be nice to be able to avoid having to weed through low-quality studies and simply wait around for higher-quality studies to be completed. That would be less effort and more reliable.
But right now we are out of time.
More than 3,000 people every day are dying in India alone and it’s imperative that we use the best scientific evidence that we do have and come up with a recommendation for a course of action that has the highest likelihood of saving the most number of lives based upon the evidence at hand now.
So now we just have to evaluate every single one of these studies in depth. But if we assume that at least one of the studies must be right, our problem is now greatly simplified since all the studies were positive. So as long as we are comfortable with the belief that at least 1 in 20 studies was well done and got the right answer, no analysis is needed since they all were positive.
If we get it wrong, we can very quickly correct our mistake
Months from now, if any high-quality Phase 3 trials complete and show we are wrong, then we can correct our mistakes at that time. This has happened before; people have been known to make mistakes. But realistically, we won’t have to wait for the Phase 3 trials because if we widely deploy a solution and it ends up being wrong, we’ll find out very quickly because the stats won’t change and we’ll then correct our mistake. So there is very little downside for taking action now and acting on the limited evidence we have.
In fact, since all three of these drugs are safe and there is no evidence that, when given early, they make the disease worse, the worst downside is the embarrassment of being wrong. On the other hand, if we stick to our guns on not recommending treatment, the worst downside is the unnecessary loss of life of hundreds of thousands of people.
So this isn’t a close call. The sooner we start ignoring these unjustifiable recommendations of the NIH and WHO, the sooner we will start saving more lives all over the world.
A NEUTRAL rating is interpreted by the world as “DO NOT USE” in practice
The NIH and WHO could argue that their treatment guidelines are practice guidelines and as such, the bar is and should be very high to get a recommendation. If a treatment with sub-optimal evidence is put on the guidelines, and later turns out to be incorrect, it would tarnish the reputation of the NIH and WHO as a trustable Gold Standards for therapies that are absolutely proven to work.
They would also point out that their guidelines are not mandates and that doctors are free to prescribe ivermectin and fluvoxamine for COVID.
They would also point out that their job is not to maximize the number of lives saved. It is only to make recommendations if and only if there is sufficient evidence in their opinion to justify the recommendation.
All of these arguments are fair and true. But it ignores the reality of how their recommendations are interpreted by governments and public health officials worldwide.
In the real world, doctors, public health officials, the media, and the public don’t have time to do the detailed research that is summarized in this paper. Instead, they rely on the Guidelines and they all interpret a neutral position as that the drug should not be used. And a NEGATIVE rating is even worse. The bottom line is that (most) every doctor in the world says if it isn’t recommended by the NIH or WHO, we should NOT use it (except in a clinical trial if so indicated).
Examples of how a NEUTRAL/NEGATIVE rating are interpreted are quite stunning: Holland will fine doctors 150,000 Euros for prescribing ivermectin. Australia will put doctors in jail for prescribing ivermectin. Pharmacies in the US will refuse to fill your ivermectin prescription by saying it is unavailable. If you talk about Ivermectin or HCQ as a treatment for COVID on YouTube, that is a violation of the YouTube Guidelines and doctors have had their videos removed, their channels frozen, and their existing videos demonetized. If you mention that these drugs work against COVID, Medium will revoke your account for life and remove all your content. If you try to tell your friends on Facebook that you are going to be featured on 60 Minutes talking about fluvoxamine, Facebook will remove the post and tell you your account will be suspended if you do anything like that again. If you try to send a private email to your contacts to let them know about the interim results of the Together Trial, SendGrid will cancel your account, remove the links in your message, delete all your contacts, and delete your unsubscribe list all before even checking with you to give you a chance to appeal.
India’s top medical officials point to the neutral/negative NIH guidelines to justify their position that there are no useful early treatments for COVID (other than the monoclonals). Brazil’s mainstream media uses the NEUTRAL/NEGATIVE positions on these drugs to teach the Brazilian public to avoid early treatment because there are no treatments that are proven to work and early treatment is dangerous. So these NEUTRAL and NEGATIVE ratings from the NIH and WHO have consequences.
Imagine going to your doctor and asking about HCQ, ivermectin, and fluvoxamine and the doctor tells you, “These drugs are not recommended by the WHO, NIH, or FDA for treating COVID and so I will not prescribe them.” That’s essentially what the NIH and WHO is telling the world.
A NEUTRAL recommendation would only be appropriate if half the studies showed a benefit and half the studies showed harm. You’d have to have a NEUTRAL position in that case and be perfectly justified. I’d even write a short op-ed on how they got it right.
But that’s not the situation we are in today. We don’t have a 15/15 win/loss record. We have a 29/0 win/loss record in HCQ and a 20/0 win/loss record for ivermectin for early treatment and the WHO tells doctors “do NOT use it.” Really?
If 29/0 win/loss ratio means “do not use,” then what will it take to get a positive recommendation?
Each recommendation has a letter grade and a numeric grade:
- Rating of Recommendations: A = Strong; B = Moderate; C = Optional
- Rating of Evidence: I = One or more randomized trials without major limitations; IIa = Other randomized trials or subgroup analyses of randomized trials; IIb = Nonrandomized trials or observational cohort studies; III = Expert opinion
If the NIH changed its recommendation on these three drugs to RECOMMEND FOR and they gave it a B or C recommendation rating with a IIa evidence rating, we’re done.
This would effectively communicate to the world that “we don’t yet have the phase 3 studies we’d normally like to see, but it’s clear that taking these three drugs leads to better outcomes than not taking the drug. We reserve the right to change our guidance in the future as we learn more.”
The alternate viewpoint
One scientist/physician who I have the highest respect for wrote this to me:
I think very likely that ivermectin and fluvoxamine have benefits, but there are some limitations of existing studies. I agree further studies are needed and that it is important to do them. I don’t think it is unethical because we do still need more confirmation of the treatment effects and also because even for people on placebo there can be advantages for the person participating in the study. For example, we monitor people closely and advise them to go to hospital when appropriate. That in itself may save some lives, even if people are taking placebo. For those who don’t wish to take the risk of being on placebo and want to see if a doctor will just prescribe them a drug, that is their choice. But to me, I think the ideal situation would be to participate in a trial so that there is potential to benefit others in terms of the knowledge gained. If we stopped all the studies before the treatment effects are fully proven, we’d take away the opportunity to clarify the effects of the treatments, and we would not allow people the potential choice to receive their treatment in a way that has potential to benefit the whole world due the knowledge gained.
I respect that point of view but my argument is that the near impossibility of these drugs not working combined with the failure of anyone to come up with any kind of plausible alternative explanation for any of the observational studies, randomized studies, and anecdotal reports all argues for using them now for saving lives and observing the reduction in deaths after these drugs are deployed. Although this approach deprives the medical community of the “clean data” they want to see the exact effect size of the drug, I would argue that saving lives now is more important and these phase 3 trials take about a year to get results. So the “balance of hardships” weighs clearly in favor of deploying the drug now. This is why the ICMR made the right decision to include both ivermectin and inhaled budesonide in their guidance.
If lives weren’t on the line, my friend’s position might be reasonable. But that’s not the case here. Note that her argument never states that her approach will minimize the number of lives lost. There’s a reason she didn’t say that: it doesn’t.
While she could argue that waiting for more data might minimize the # of lives lost in the long term because docs will be convinced at a higher rate at that point in the future, that’s a speculative argument; I could easily argue that when people try it now and see results, others will quickly follow suit.
Either the drug works, doesn’t work, or causes harm. Based on the observed data, there is absolutely no question that the hypothesis that fits the data the best is the hypothesis that the drug works. Even she admits that there is more than a 90% chance that the effect is real. Therefore, using it until proven otherwise, is the course of action that is most likely to maximize the number of lives saved today.
In short, if I offered you a choice of envelopes, one that has 1 lottery ticket in it, and a second envelope with at least one ticket but possibly 10 lottery tickets, which one do you pick?
Cognitive dissonance coping techniques
The arguments in this article will be uncomfortable for many people, especially those who hold the belief that the NIH and WHO can do no wrong.
If people ask you what you think about this article, here are some ways you can respond:
- Tell them you read the article, and agree that yes, all the effects were positive, but since each and every study can be discredited in one way or another, it means that there is no data. 20 bad studies is 20 x 0. This is the most popular technique because once you can ignore the evidence you’re done… there is therefore no effect so the drug shouldn’t be used since all drugs have risks.
- Point out that because the author isn’t a doctor, it’s not worth even discussing. Ad hominem attacks are useful because you can avoid having to argue the merits.
- Point out that the site relied upon, c19early.com, was assembled by someone who won’t disclose their identity (for fear of retribution) and because the site is dynamic, it can’t be peer-reviewed, so it cannot be trusted. Then you hope they don’t check the site and find out everything on the site is actually accurate.
- Point out that the paper in Lancet that proved hydroxychloroquine worked was retracted. This is of course completely backwards, but it will fool most people into believing that you are right since most people will trust you (and some doctors actually believe this).
- Tell them, the reason HCQ was not recommended is not because it didn’t work, but because there are more effective early treatments approved by the WHO, so the WHO didn’t want people using the less effective treatments.
- Tell them the article was too long and you didn’t have time to read it yet, but you’ll get back to them later when you are less busy. Then be sure to stay busy.
- Point out that the WHO and NIH are just their opinions and everyone is entitled to their opinion. These opinions are supposed to be based on evaluation of top quality evidence so when no evidence is available, they have to give a neutral rating, even if it means lives are lost. Unfortunately, this argument isn’t that good because it is not consistent since if the studies are all defective, that would argue for a NEUTRAL rating until there are high-quality studies.
- Point out that Merck said ivermectin shouldn’t be used for COVID and they are trustworthy because they have everything to lose since they make the drug. Hope that nobody finds out that Merck is pursuing more profitable drugs that are not generics and a working generic would negatively impact their revenue potential.
- Point out that pharmacies will refuse to honor prescriptions and drug companies will cut off the supplies of ivermectin. Thus even if everything in the article is correct, it won’t change anything.
- Simply refuse to read it. This is what leading infectious disease experts have done when I have requested they read it and tell me if they found any errors. They can’t go against the party line or their future research won’t get funded. Institutions have long memories.
- Tell them “Look it happens all the time that Phase 2 studies are reversed Phase 3 studies. We have to be careful here.” If they subsequently ask “Really? When was the last time you had 29 positive studies in a row and the Phase 3 study reversed it?” then just say, “I haven’t got time to find all the studies” and walk away.
Summary
If we want to minimize fatalities, we should make decisions based on the best evidence on the table today and pick the option that is most likely to minimize fatalities.
This is not a close call at all. The evidence on the table is both consistent and compelling for all three drugs. The consistency of the data we have in hand, and the confirmation in anecdotal reports from hundreds of doctors and thousands of patients, makes it far more likely that the drug works as claimed. Nobody has posited an alternative explanation that can fit even a small subset of the evidence.
If we are wrong in recommending the drug, no harm is done. But if we are wrong in not recommending the drug, we’ve unnecessarily cost the lives of millions of people.
These three drugs are not NEUTRAL or NEGATIVE. They are POSITIVE. These drugs can and will save lives if we expressly allow doctors to deploy them now.
Today, public confidence in the NIH is headed to an all-time low. This article has highlighted some of the reasons why. Their positions on these three drugs are not defensible. Even though this is an issue of great public interest, I fully expect both organizations will decline a public debate with the world’s experts on each of these drugs.
The reason they will decline is they know that they would lose such a debate. Badly. But they will make up some excuse as to why, even with thousands of people dying daily in India alone, that they are simply too busy to defend their recommendations in a neutral open forum.
I know from talking to the doctors using these drugs today that we can drastically reduce hospitalization, death, and long-haul COVID is to treat every infected patient (regardless of age and risk factors and symptoms) as soon as possible with just two drugs: ivermectin and fluvoxamine. I am not aware of a single person who received the combination of just those two drugs early (within 24 hours of their very first hint of COVID symptoms) who was hospitalized, died, or ever developed long-haul COVID. This is based on unpublished efficacy data from over 600 outpatients treated by several physicians in multiple countries and points to an efficacy signal from the combination without untoward toxicity (there are no drug interactions between the drugs). After the combination was added to the FLCCC protocols, there have been no adverse reports from the combination.
I urge doctors: if someone tests positive, do not wait for symptoms before giving treatment; that’s like waiting for your entire house to be on fire before calling the fire department. COVID should be treated just like David Ho said we should treat HIV: fast and hard. And just like it took many years to learn that lesson for HIV, it will unfortunately take the same amount of time with COVID for doctors to realize that this virus should be treated the same way as that virus. There has never been a virus in human history where there are better results by treating it late. Old habits die hard.
Just like doctors should treat COVID without waiting for symptoms, the NIH and WHO should not wait for more data. The world is on fire and needs action now. A fire captain never asks for large randomized trials before rendering a decision on the best strategy for combating a fire; she makes the best decisions to minimize death and disability based on the evidence in hand, even if that evidence isn’t perfect. The WHO and NIH should do the same. The sooner they adjust their recommendations consistent with maximizing the number of lives saved, the better.
Steve Kirsch is a high-tech serial entrepreneur based in Silicon Valley. He has been a medical philanthropist for more than 20 years. When the pandemic started, he left his day job at M10 and started the COVID-19 Early Treatment Fund (CETF), which funds researchers from all over the world running outpatient clinical trials on repurposed drugs. CETF funded David Boulware’s trials on hydroxychloroquine and the Phase 2 and Phase 3 fluvoxamine trials, among many other research projects. He was recently featured on 60 Minutes, which highlighted his work with fluvoxamine. He has no conflicts of interest; his objective is to help save lives. In 2003, Hillary Clinton presented him with a National Caring Award. He wrote this article to share some of what he has learned over the past year about the failure of evidence-based medicine during a pandemic in the hopes that people will realize their mistakes and change their views.
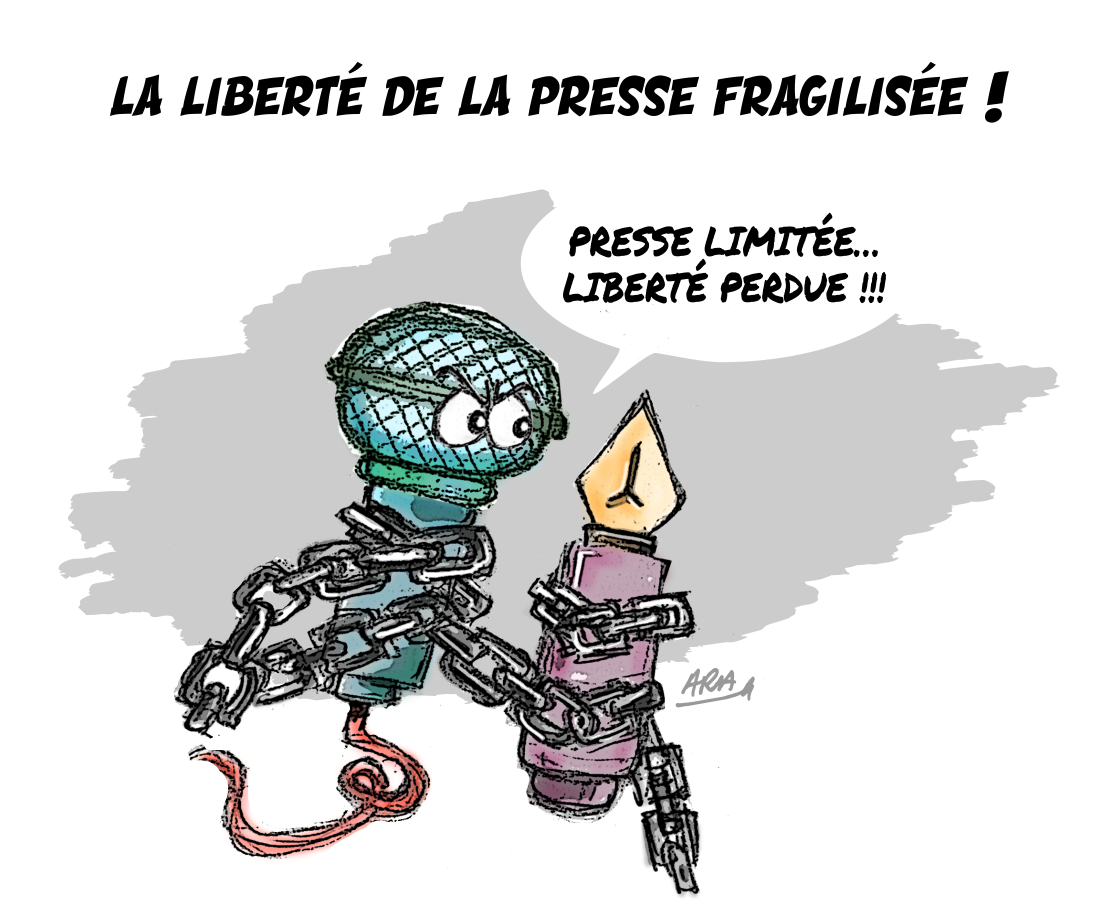
L'article vous a plu ? Il a mobilisé notre rédaction qui ne vit que de vos dons.
L'information a un coût, d'autant plus que la concurrence des rédactions subventionnées impose un surcroît de rigueur et de professionnalisme.
Avec votre soutien, France-Soir continuera à proposer ses articles gratuitement car nous pensons que tout le monde doit avoir accès à une information libre et indépendante pour se forger sa propre opinion.
Vous êtes la condition sine qua non à notre existence, soutenez-nous pour que France-Soir demeure le média français qui fait s’exprimer les plus légitimes.
Si vous le pouvez, soutenez-nous mensuellement, à partir de seulement 1€. Votre impact en faveur d’une presse libre n’en sera que plus fort. Merci.